Learn how the Bridge Program applies to NYCE PPO, Large Group, and ASO plan members in 2026.
Search
Popular Tasks
EmblemHealth Announces Initiatives to Reduce Prior Authorization
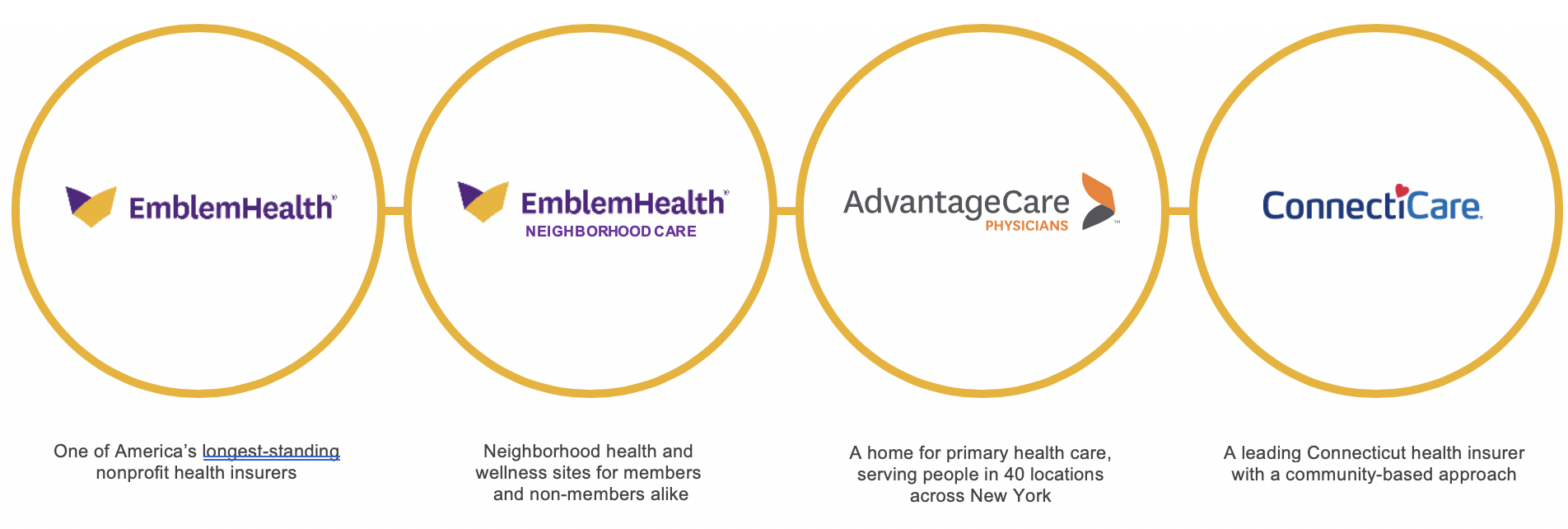
EmblemHealth has a mission to create healthier futures for our customers and communities. We fulfill that mission by working closely with our networks of medical professionals delivering care. This collaboration informs everything we do. That is why we have formed a unique partnership with AdvantageCare Physicians of New York (ACPNY), one of the largest medical groups in the New York City area. In effect, we are a health plan and a physician practice working together every day to bring high-quality and affordable care to the individuals we serve.
EmblemHealth will soon be taking important steps to make sure doctors, nurses, pharmacists, and other clinicians can more fully devote their attention to providing the care people deserve. As part of our overall transformation and introduction of new technology, we are significantly reducing the number of procedure codes that need our approval before delivering care starting Jan. 1, 2020. Our new processes are based on national treatment standards developed by physicians and other medical professionals that establish best practices for ensuring people receive high-quality, affordable care and that science leads decision-making.
Below, we provide additional information on this important change.
The Issue
Health plans have established procedures that require physicians, nurses, and others to receive approval from the plan before the care is covered under the individual’s policy. These processes, referred to as “prior authorization,” ensure that the plan covers the most appropriate care. Unfortunately, in the health care system today there are too many instances of services being overprescribed, delivered in the most expensive settings, and bills submitted for services that do not meet patient needs. In addition to the adverse clinical, financial, and emotional impact of unnecessary care delivery, overuse causes patients to undergo unnecessary tests and stays in the hospital when they should be at home.
Research demonstrates providers often overuse services, which creates unnecessary hassles for patients and makes care less affordable. A recent survey1 found most physicians acknowledge 15% to 30% of care they prescribe is unnecessary. Another report2 appearing in The Journal of the American Medical Association (JAMA), finds waste accounts for about one out of every four dollars spent on health care in the U.S. every year, with $75 billion to $100 billion of this attributed to “Overtreatment or Low-Value Care.”
For example, more than 75 medical specialty groups including the American Association of Family Physicians, the American Pediatrics Association, and the American College of Physicians have been working since 2012 on the Choosing Wisely3 initiative, which is designed to “identify tests or procedures commonly used in their field whose necessity should be questioned and discussed”.
However, we know from our experience as a health plan and a provider that our enrollees and their clinicians often view prior authorization as burdensome. Health care researchers and clinical societies have done significant work to shine a light on best practices and ways to reduce inefficiencies in this area.
What Are We Doing?
Informed by this initiative and our ongoing work to use technology and information to fully transform our health plan, we recently reviewed our prior authorization procedures to ensure we are providing the best possible care. As a result, we are significantly reducing the number of procedures requiring prior authorization. This change affects enrollees in all our plans, including Medicaid managed care, Medicare Advantage, coverage offered through employers, and Individual Market plans on the Exchange.
These changes fall generally into the following categories:
• Acute Care Hospital Services: We have modified prior authorization based on our data analysis by identifying services that almost always get approved. These services include some major surgical procedures and common surgical procedures where patients are going to the hospital. Examples include heart valve replacement surgeries, other cardiac procedures, and other procedures listed below. We previously required prior authorization to ensure the individual had undergone less invasive procedures to improve their health. However, we have concluded that in many cases our enrollees who are prescribed these procedures have found these less invasive techniques do not cure their conditions. We will continue to review our data to allow us to find additional ways to improve care for the people we serve.
• Site of Service: We will continue to review some services to ensure that our members are receiving the right care at the right place at the right time using evidence-based criteria and ensuring requests meet quality standards. For example, studies demonstrate many health care procedures such as colonoscopies and skin lesion biopsies can be provided safely and effectively in physicians’ offices and ambulatory service centers (ASCs) at about half the cost as a hospital outpatient department. Our new processes will only require prior authorization when the services are provided in these more expensive settings.
Examples of Procedures for Which We No Longer Require Prior Authorization
| Acute Care Hospital Services | Site of Service |
|---|---|
|
|
The procedures that remain eligible for prior authorization closely follow the Choosing Wisely recommendations and other evidence-based standards. Choosing Wisely’s website identifies several examples of how hospital adherence with practices like these improved care, such as by reducing the inappropriate use of addictive benzodiazepines and significantly lowering surgical site infections4. We are confident our enrollees will benefit from this work and our ongoing, clinically driven analyses that will continue to provide the basis for our coverage policies.
Why Are We Doing This?
EmblemHealth is a nonprofit health plan. Our first interest is to our enrollees, not stockholders. That is why in addition to our close partnership with ACPNY, we also operate 12 Neighborhood Care centers located in low-income and ethnically diverse areas throughout New York City. These facilities are staffed by care navigators who help consumers through the health care and social service systems and connect them with resources to address the full range of social factors affecting their health.
Our change is motivated by these goals. By reducing the number of procedures that require prior authorization, the clinicians on the front lines of our care delivery system – the physicians, nurses, and pharmacists – will have more time to spend with their patients and to further support this goal. We are updating our provider portal to speed the authorization of those items that remain. By maintaining more streamlined health plan management tools, we can continue to help make care more affordable and accessible to the individuals we serve.
Conclusion
EmblemHealth is a different kind of health plan. We view health care as a right, not a commodity. It is our job to ensure the people of New York, Connecticut, Massachusetts, and New Jersey can exercise their rights through the availability of high-quality, affordable health care. We live this vision every day through our partnerships with physician groups like ACPNY, our focus on the social factors affecting care, and our commitment to our communities.
EmblemHealth’s decision to reduce the number of procedures requiring prior authorization starting January 1 is consistent with these goals. Our 3.1 million enrollees will know they have their clinicians’ full attention while receiving care consistent with recommendations from medical experts. Medical professionals will have more time to focus on their patients’ needs while spending less time on paperwork. We look forward to continuing to work with our partners and others to provide high-quality, affordable care to the individuals we serve.
1 Lyu H, et al., “Overtreatment in the United States”. PLOS One (Sept. 6, 2017).
2 Shrank, William H., MD, MSHS et. al., “Waste in the US Health Care System: Estimated Costs and Potential for Savings”. JAMA. 2019;322(15):1501-1509 (October 7, 2019).
3 Please see http://www.choosingwisely.org/ for more information.
4 Please see examples found here and here.


