Learn how the Bridge Program applies to NYCE PPO, Large Group, and ASO plan members in 2026.
Search
Popular Tasks
Veradigm Risk Adjustment
What is Risk Adjustment?
Risk adjustment is a process that considers member demographics and health status to assess the relative risk whether a member may incur medical expenses above or below an overall average within a defined time frame. Diagnoses are collected from submitted claims and their specificity helps drive risk categorization. Patients with serious and/or multiple health conditions tend to have higher risk scores than patients who do not. Accurate risk categorization assists in the financial forecasting of future medical need and helps to identify members for disease management interventions.
Risk adjustment programs are developed and managed by government agencies, as introduced by the Medicare Modernization Act of 2003. These programs were created to serve all eligible members of the public, so that health insurance companies cannot discriminate or purposely insure only a certain demographic of members with a limited range of expected health care costs. Risk adjustment is also critical for ensuring adequate compensation to health insurance companies, so they are able maintain coverage and access to care for beneficiaries likely to incur higher-than-average costs.
Patients
- Identifies patients that would benefit from a treatment plan for their diagnoses.
- Can participate in Care Management programs offered by EmblemHealth.
- Stay engaged in their health.
Providers
- Capture and understand their patients' full burden of illness to better manage health care outcomes.
- Earn additional reimbursement.
EmblemHealth
- Receives proper reimbursement from the Centers for Medicare & Medicaid Services (CMS) to cover the costs derived from the conditions of the patient.
EmblemHealth uses claims coding data to find possible instances of incorrect and/or missing diagnoses that require review, correction, and/or validation. Once these situations are identified, the charts for those members are reviewed.
Providers must submit accurate and specific claims diagnosis coding and maintain detailed medical documentation, as it is critical for risk adjustment. The risk adjustment model relies on ICD-10-CM coding to represent the member’s health status, not just CPT procedure codes. Records are used for validation. Physicians are the main source of information for the risk adjustment model.
Any primary care provider (PCP) who cares for EmblemHealth members enrolled in these products:
- New York State of Health (NYSOH) Marketplace
- Medicare HMO
- Medicaid
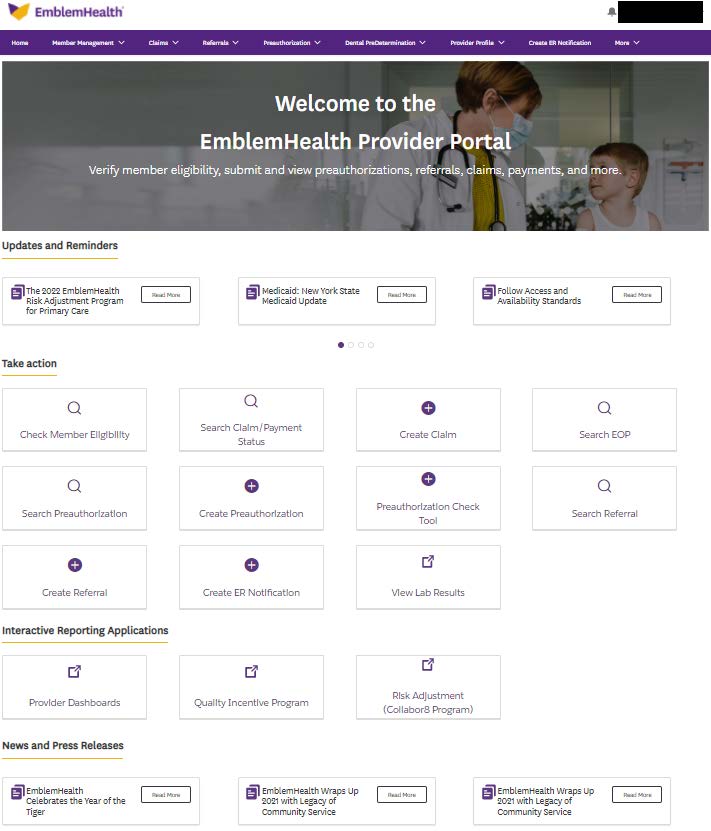
You can access and submit your correct claims and medical records via the secure Collaborate web-based tool by simply registering on EmblemHealth’s Provider Portal at emblemhealth.com/providers. Once you register/sign on to EmblemHealth’s Provider Portal, select the portal page entitled Risk Adjustment (Collaborate Program) and then click on the hyperlink entitled Risk Adjustment (Collaborate Program). By clicking “Continue,” you will be taken right into theCollaborate tool without having to separately register/sign on.
By submitting a claim to EmblemHealth and completing a compliant Provider Alert in the secure Provider Portal along with the supportive progress note(s) in Collaborate, you can receive the following:
Medicare HMO Members
Completed Alert with attached Progress Notes = $150 per member
Completed Alert with attached Progress Notes prior to July 1 = an additional $75 per member
Medicaid Members
Completed Alert with attached Progress Notes = $40 per member
Completed Alert with attached Progress Notes prior to July 1 = an additional $20 per member
NYSOH Marketplace Members
Completed Alert with attached Progress Notes = $100 per member
Completed Alert with attached Progress Notes prior to July 1 = an additional $50 per member
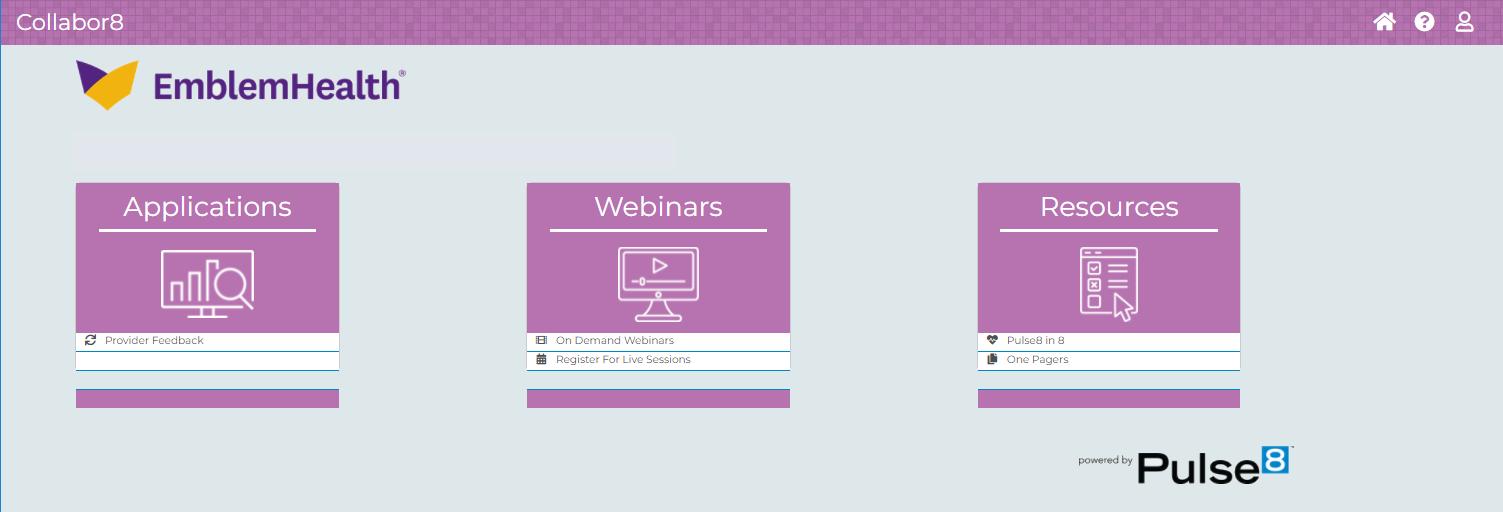
EmblemHealth partners works with Veradigm’s Collaborate to provide our providers with a web-based tool that supports improvements in documentation, quality, and risk score accuracy. This tool allows providers and their staff to access helpful online risk adjustment resources, easy-to-use dashboards, and provider alerts for your EmblemHealth members.
EmblemHealth works with Veradigm to establish a risk adjustment program to:
- Help monitor the patient population.
- Provide important information relating to the improvement and quality of care.
- Increase provider engagement.
- Increase accuracy and completeness of data submissions to achieve more accurate risk adjustment factor scores.
How to access the Collaborate/Veradigm tools.