Effective Jan. 1, 2026 New York City employees, pre-Medicare eligible retirees, and their dependents are now offered the New York City Employees PPO plan (NYCE PPO), a health benefit plan delivered through a partnership between EmblemHealth and UnitedHealthcare.
What’s changing?
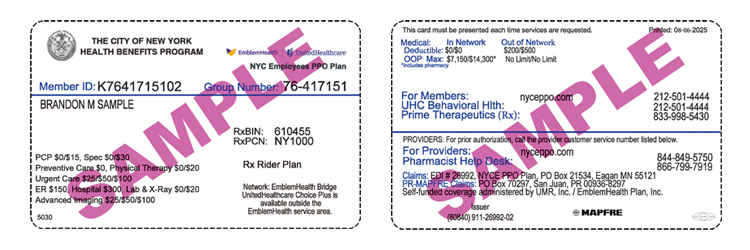
- The member ID card: NYCE PPO members now have one card for both facility care and professional care.
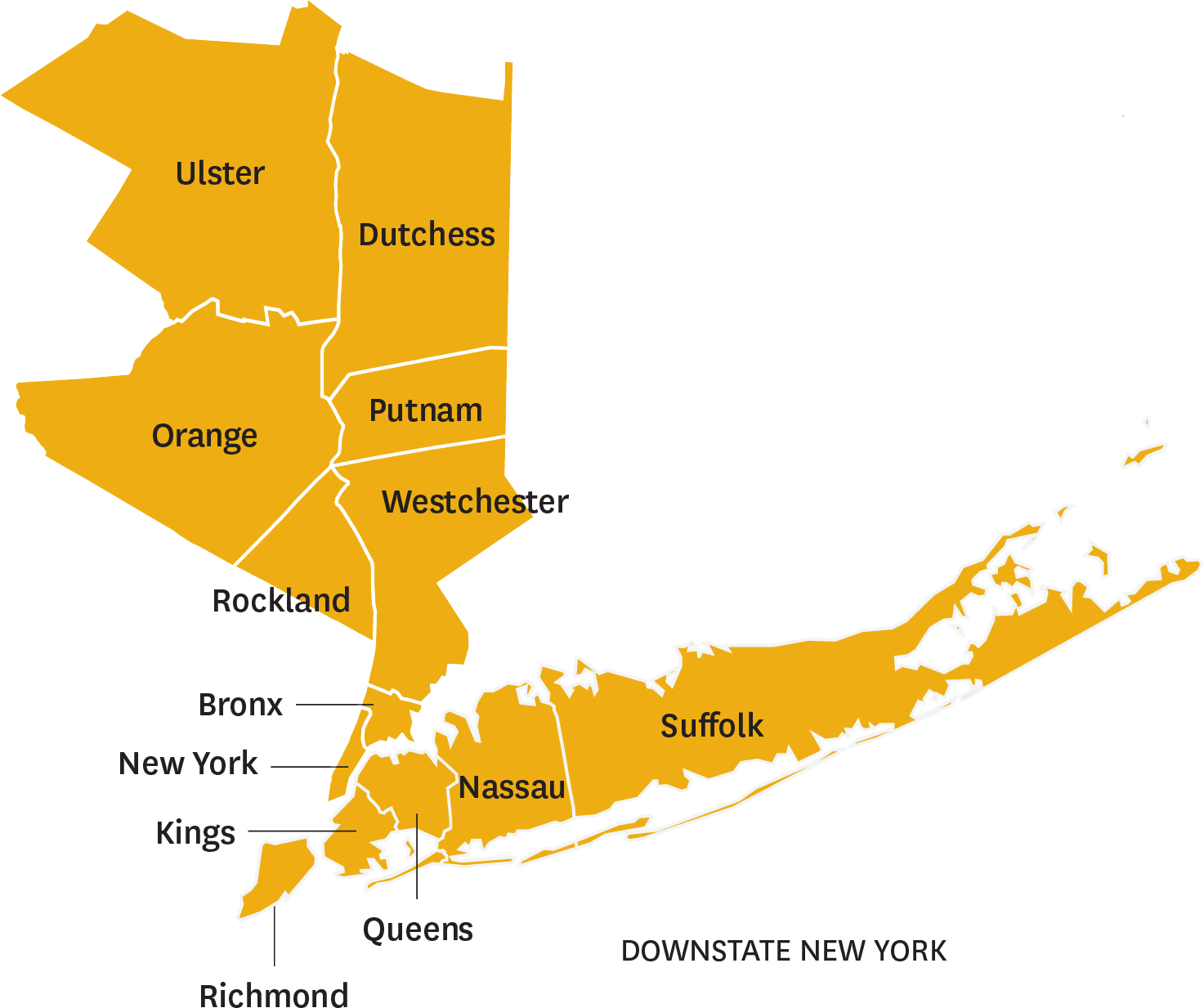
- Who’s in-network: NYCE PPO is a partnership between EmblemHealth and UnitedHealthcare. The plan uses the EmblemHealth Bridge Program for all facilities and providers in the 13 counties in lower New York state and the UnitedHealthcare national Choice Plus network outside these counties (in the remaining New York state counties and nationwide).
- The portal: EmblemHealth and UnitedHealthcare providers have a single, secure portal powered by UMR (the third-party administrator that’s part of the same family of companies as UnitedHealthcare).
We have created this list of Frequently Asked Questions (FAQs) to help answer some of the most pressing queries you may have about this plan.